For many people, alcohol is an accepted part of their daily diet. In the US, over 60% of adults admitted to regularly consuming alcoholic beverages like wine and beer.
Most of us understand that drinking alcohol, particularly when taken in excess amounts beyond what’s recommended, can have adverse effects on our health.
From mental health concerns like addiction and behavioral issues to life-threatening scenarios (e.g., drunk driving), there’s a range of harmful consequences that could arise from frequent drunken stupors.
Our gut health is the first to take the brunt after heavy drinking. It’s common for people to feel sick after a night of partying and cocktails. But how much damage does alcohol actually do to your digestive system? How to restore gut health after alcohol abuse?
Here’s everything you should know about how excessive alcohol consumption damages your gut health and how to nurse your microbiome back to health.
Table of Contents
How Alcohol Harms Your Gut Health
Our everyday choices impact our bodies. And regardless of the amount of alcohol you drink, it carries certain health risks you may want to consider.
For most people, drinking beverages with ethanol in moderate amounts is generally safe. However, the dangers increase as the amount you consume goes up, potentially harming your digestive health.
Here are some of the ways alcohol use can damage your intestinal health:
Alcohol Alters Your Gut Microbiome
Your microbiome consists of the non-human inhabitants inside your body. But before you freak out, they’re mostly harmless, made up of trillions of good gut bacteria and other microbes.
The healthy balance of these welcome inhabitants supports several vital functions in your body, helping the immune system, boosting metabolism, fighting infection, regulating inflammation, and helping liver functions.
Your diet, however, has a massive impact on the microbiome’s balance. Whatever you ingest can affect everything—from your oral microbiome to your digestive system.
Alcohol affects the beneficial bacteria and microbes inside your stomach. It disrupts the balance (homeostasis) of the gut flora and can lead to dysbiosis, where everything goes haywire, increasing your gut’s vulnerability to various health conditions.
Metabolizing large amounts of alcohol also increases metabolite production, substances that function as signals to your gut, liver, and blood.
Some of the metabolites produced from digesting alcohol can be toxic, overwhelming the gastrointestinal tract (GI), stomach lining, and the liver, a condition called gut-deprived inflammation.
Leaky Gut Syndrome
Leaky gut syndrome is a medical condition characterized by a string of digestive issues, including heartburn, bloating, gastritis, and diarrhea. It may manifest alongside symptoms like headaches, fatigue, and skin problems.
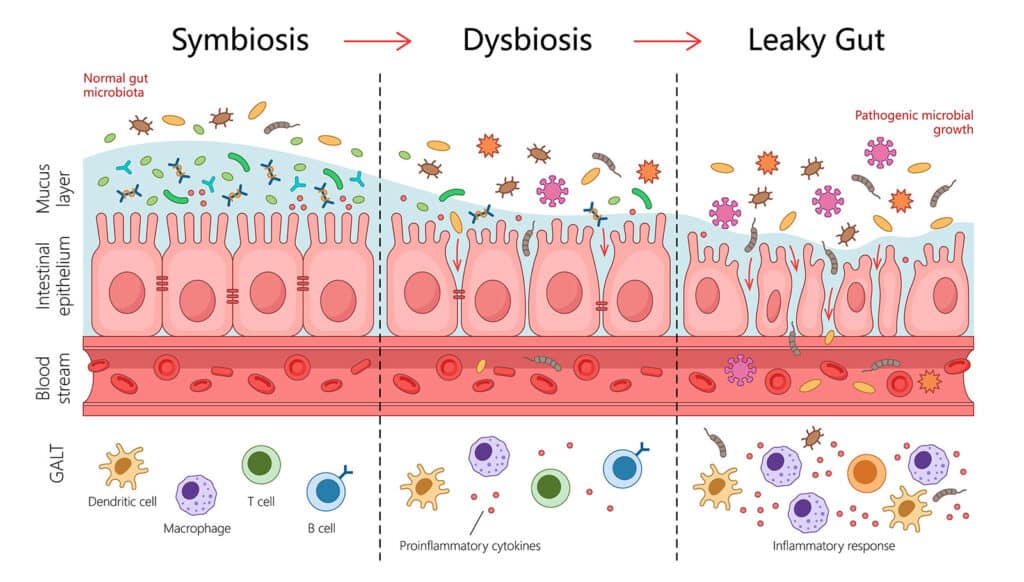
One of the effects of alcohol is that it damages the gut lining’s protective mucus layers. When this happens, the microbes will start to chip away at the intestinal wall that divides the stomach and the rest of your body.
The following deterioration increases the digestive tract’s permeability, resulting in leaky gut syndrome. Repeated irritation of the stomach lining also increases the likelihood of ulcers developing.
Increased Risk of Liver Disease
Besides your digestive health, several vital organs, like the liver, may also suffer from heavy alcohol use. Prolonged exposure to the substance increases your likelihood of contracting various liver diseases, such as cirrhosis and cancer.
As you know, the liver serves an essential purpose besides aiding digestion. It’s the primary organ responsible for blood filtering, drug metabolizing, and receiving nutrients for nutrient absorption.
Excessive and prolonged alcohol intake can result in a number of liver diseases, such as:
- Hepatic steatosis, or fatty deposit buildup in the liver
- Severe liver inflammation or alcoholic hepatitis
- Scarring in the liver tissue, referred to as cirrhosis
Most heavy drinkers develop a fatty liver, and about a third of people suffering from alcohol use disorder (AUD) contract hepatitis. A significant portion (10% to 20%) of chronic drinkers are also likely to be diagnosed with cirrhosis after 10 or more years.
Greater Vulnerability to Pancreatic Diseases
Like the liver, the pancreas is a crucial organ that aids several invaluable bodily functions. Its job involves producing enzymes that aid digestion and regulating blood sugar levels by releasing insulin.
However, when alcohol is present, the pancreas metabolizes the ethanol and produces toxic byproducts that could be harmful to the pancreatic or bile ducts.
Enzymes that should be released into the digestive tract can also start piling up and eat the pancreas on the inside. This abnormality can cause an agonizing inflammation of the organ called pancreatitis.
Pancreatitis as a result of alcohol is found to be prevalent in people who drink above the recommended daily alcohol intake for five years or longer.

How to Heal Your Gut After Alcohol Abuse
The good news is that while some co-occurring disorders alongside AUD can persist for several years, an imbalance in the gut microbiome can be fixed if you make an effort to live a little more health-conscious.
Here’s a list of expert medical advice to recover a healthy gut after years of alcohol consumption:
Sleep Regularly
As surprising as it sounds, your sleeping pattern massively affects your body’s microbiome. Our gut microbiota follows our natural circadian rhythm and fluctuates accordingly. So, the more consistent your sleep routine, the healthier your gut becomes.
An irregular sleeping schedule, on the other hand, disrupts that natural cycle, increasing the risk of gut inflammation and other digestive issues.
Drink Plenty of Water
Hydration is just as crucial to your micro tenants’ overall health. Water is key to ensuring your food moves from the small intestine to the large intestine properly and is a key ingredient for digestion.
Experts recommend drinking 3.7 liters of water for men and 2.7 liters of water for women every day to maintain a sufficiently hydrated gut. Additionally, incorporating water-rich fruits and vegetables like watermelon, cucumber, and oranges into your diet adds essential vitamins, minerals, and antioxidants.

Opt For a Healthier Diet
As we already said above, whatever you eat directly impacts your gut. Unfortunately, the Western diet often consists of plenty of sugar, animal protein, and fat, which are shown to decrease good bacteria in the stomach.
Instead of a slice of pizza, opt for a healthier diet consisting of veggies, fruits, and whole grains. Eat less red meat and dairy products to increase your gut’s good bacteria count, particularly Lactobacillus and Bifidobacterium.
Add Probiotic Supplements to Your Meal Plans
If you’re experiencing symptoms of an imbalanced microbiome, your healthcare provider may recommend probiotic supplements to improve your condition.
Probiotics are food and beverage products that contribute beneficial bacteria and yeasts to your gut’s friendly microbes.
Another way to invigorate your microbiome is to consume lots of prebiotics. These are indigestible fibers in raspberries, lentils, and beans. Instead of adding more, prebiotics boost gut health by supporting the existing microbiota.
Go Out and Exercise
Regular exercise has been proven to aid your digestive tract’s health, as found in a 2021 research study with athletes. As simple as a 30-minute workout or running can significantly improve gut microbial diversity.
It’s important to remember that your digestive tract is a muscle. Working out and moving your entire body regularly benefits your muscles, even your gut.
Moreover, going out into the world, playing on the dirt, and lounging on the grass exposes your body to natural microbes in the environment. This can help replenish a diminished good bacteria count and encourage microbial diversity in your digestive system.
Reduce Stress
Stress is a killer of good gut bacteria. In one recent animal study, experts concluded that prolonged exposure to elevated stress significantly decreases your gut’s beneficial bacteria and increases bad ones.
Help your gut by de-stressing and avoiding stressors and instances where you’ll experience anxiety. Chronic stress is particularly problematic as it significantly alters your intestine’s permeability.

Final Thoughts: Breaking Free From Alcohol Use
Breaking free from the vicious cycle of alcohol use is the ultimate answer to resolving its adverse health consequences.
If you or any of your loved ones are experiencing gut health problems due to heavy and problematic alcohol consumption, getting professional help is the best way forward.
Garden State Treatment Center is a trusted drug and alcohol rehab in New Jersey with experts dedicated to helping people suffering from AUD and SUD and their co-occurring symptoms, including gut health disorders.
Contact Garden State Treatment Center and start your sober days now!
References
- https://www.pewresearch.org/short-reads/2024/01/03/10-facts-about-americans-and-alcohol-as-dry-january-begins/
- https://www.genome.gov/genetics-glossary/Microbiome
- https://www.healthline.com/health/dental-and-oral-health/what-does-alcohol-do-to-your-teeth
- https://www.niaaa.nih.gov/publications/alcohol-metabolism
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5513683/
- https://www.mayoclinic.org/diseases-conditions/alcoholic-hepatitis/symptoms-causes/syc-20351388
- https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/basics-defining-how-much-alcohol-too-much
- https://alcohol.org/co-occurring-disorder/
- https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256
- https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-017-1175-y
- https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.637010/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7213601/
Published on: 2025-04-27
Updated on: 2025-04-27



